Urinary incontinence is a widespread condition that affects millions across the United States and beyond. This guide explains its types, causes, and available treatments. You will also need the help of a physical therapist and take proactive steps toward regaining control and confidence in your life.
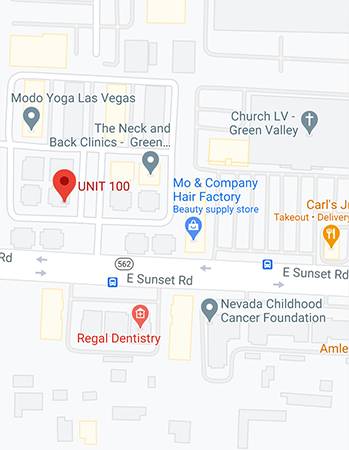
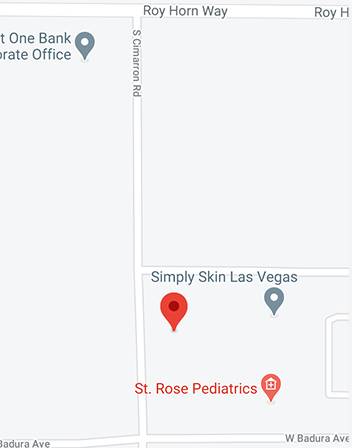
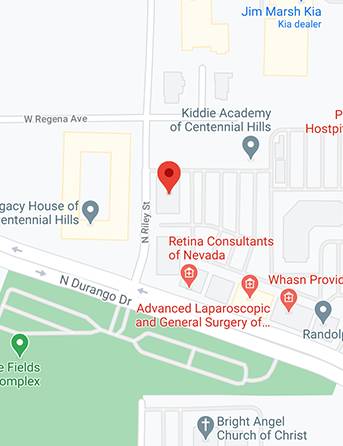
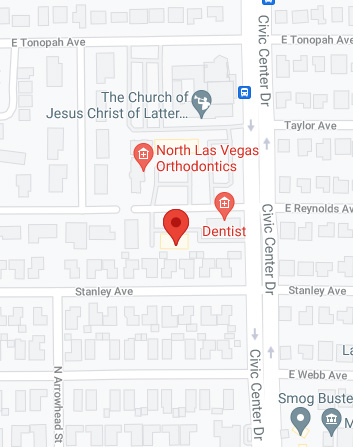
At Suarez Physical Therapy, we are dedicated to helping you regain your quality of life. If you seek a therapist in Las Vegas, we will help manage urinary incontinence and discover effective treatments.
What Does Urinary Incontinence Mean?
Urinary incontinence happens when your urine leaks. In the US, over 13 million patients suffer from urinary incontinence. Types of urinary incontinence include the following:
Stress Incontinence
Stress incontinence occurs when there is an involuntary loss of urine during activities that put pressure or stress on your bladder and pelvic floor muscles.
Stress incontinence is often triggered by coughing, sneezing, laughing, lifting heavy objects, or engaging in high-impact exercises. These activities can lead to a sudden, unexpected leakage of urine.
Women's primary cause of stress incontinence is the weakening of the pelvic floor muscles and the supportive tissues that hold the bladder in place. This weakening can occur due to various factors, including pregnancy, childbirth, and hormonal changes during menopause. In men, prostate surgery can also contribute to stress incontinence.
The most apparent symptom of stress incontinence is the leakage of urine when pressure is exerted on the bladder. However, it's essential to note that this condition can vary in severity, with some individuals experiencing minor leaks and others facing more significant challenges.
Beyond the physical discomfort, stress incontinence can considerably impact your daily life. If not properly managed, it can lead to embarrassment, social withdrawal, and a decreased quality of life. The good news is that effective strategies and treatments are available to address stress incontinence. Physical therapy is crucial in strengthening the pelvic floor muscles, improving bladder control, and reducing or eliminating leakage episodes.
Urge Incontinence
Urge incontinence, often called "overactive bladder," is characterized by a sudden, intense urge to urinate, followed by an involuntary loss of urine. It can happen at inconvenient times and can be challenging to control.
One of the hallmark symptoms of urge incontinence is a frequent and intense need to urinate. You may rush to the bathroom even when you've emptied your bladder.
Urge incontinence can result from various factors, including muscle or nerve damage, certain medical conditions, or simply an overactive bladder muscle. Neurological disorders such as Parkinson's disease or multiple sclerosis can also contribute to this condition.
Specific triggers can worsen urinary incontinence, such as drinking caffeine and alcohol or consuming spicy foods. Stress and anxiety can also exacerbate the urgency and frequency of urination.
Urge incontinence can have a significant impact on your daily life. It may limit your social activities and lead to anxiety about finding restrooms quickly. This can, in turn, affect your overall quality of life.
Mixed Incontinence
Mixed incontinence is characterized by experiencing symptoms of both stress and urge incontinence simultaneously. Individuals with mixed incontinence may involuntarily lose urine during physical activities or when sneezing and coughing (stress incontinence) and experience sudden, strong urges to urinate (urge incontinence).
Mixed incontinence can present a unique challenge as it combines the characteristics of two distinct types of urinary incontinence. This often leads to a more complex and disruptive experience for individuals.
The causes of mixed incontinence can vary. Some individuals may have weakened pelvic floor muscles, making them susceptible to stress incontinence, while others may have an overactive bladder, contributing to urge incontinence. Understanding the underlying factors is essential for effective management.
Triggers for mixed incontinence can include activities that provoke stress, such as lifting heavy objects, and situations that exacerbate urge incontinence, like drinking caffeinated beverages. Managing these triggers is crucial to symptom control.
Functional Incontinence
Functional incontinence occurs when a person has the physical capability to control their bladder but faces obstacles that prevent them from reaching the restroom promptly. These obstacles are often related to cognitive or physical impairments rather than a malfunction of the urinary system itself.
Functional incontinence is typically associated with conditions that affect mobility, cognition, or both. Common causes include advanced age, dementia, physical disabilities, and cognitive impairments.
Individuals with functional incontinence may find it challenging to navigate their environment, leading to involuntary urine loss. For example, someone with severe arthritis may struggle to unbutton their pants quickly enough, while someone with cognitive impairments may forget the route to the restroom.
This type of incontinence can significantly impact an individual's quality of life. It may result in embarrassment, social isolation, and a loss of independence, as those affected may require assistance managing incontinence.
Urinary Frequency
Urinary frequency refers to the condition in which an individual experiences an increased need to urinate, often resulting in more frequent trips to the restroom than what is considered typical. This phenomenon can be perplexing and sometimes disruptive to daily life.
Several factors can contribute to urinary frequency, which may vary from person to person. Some of the common causes include:
- Certain foods and beverages, such as caffeine and spicy foods, can irritate the bladder and increase urinary frequency.
- Urinary tract infections (UTIs) can cause a frequent urge to urinate, along with other symptoms like pain and discomfort.
- Some medications, including diuretics and certain antihypertensive drugs, can increase urine production and lead to more frequent urination.
- Conditions like diabetes and overactive bladder syndrome can contribute to urinary frequency.
Causes of Urinary Incontinence
Day-to-day activities, habits, physiological issues, and other conditions could cause urinary incontinence.
Temporary Urinary Incontinence
Brief episodes of involuntary urine leakage characterize temporary urinary incontinence. Unlike persistent incontinence, often linked to underlying medical conditions, temporary incontinence is typically associated with specific triggers or situations.
Below are factors that cause temporary urinary incontinence:
- Certain medications can disrupt normal bladder function and lead to temporary incontinence. This includes diuretics, which increase urine production, and medications like sedatives, muscle relaxants, and some antihypertensive drugs that can affect bladder control.
- Both alcohol and caffeine are known diuretics, meaning they prompt the body to produce more urine. Consuming excessive amounts of these substances, especially close to bedtime, can result in temporary urinary incontinence.
- Infections in the urinary tract, such as UTIs, can irritate the bladder lining and cause symptoms like frequent urination and sudden urges to urinate, which may lead to incontinence.
- Severe constipation can pressure the bladder and nearby structures, causing disturbances in normal urinary function. Treating constipation often alleviates the associated incontinence.
- High-impact activities like jumping or running can stress the pelvic floor muscles. This stress can lead to temporary incontinence, particularly in women.
Persistent Urinary Incontinence
Persistent urinary incontinence is a chronic condition characterized by ongoing and often involuntary urine leakage. Unlike temporary incontinence, which is usually triggered by specific factors, persistent incontinence is typically linked to underlying medical or physiological factors. These causes are as follows:
- Pregnancy can lead to urinary incontinence due to the increased pressure on the bladder and pelvic floor muscles. Hormonal changes during pregnancy can also affect bladder control. In many cases, this type of incontinence resolves or improves after childbirth.
- Vaginal childbirth can cause damage to the pelvic floor muscles and nerves, increasing the risk of persistent urinary incontinence. Trauma during delivery or the use of forceps may contribute to this condition.
- Aging is a significant risk factor for urinary incontinence. The natural aging process can weaken the pelvic floor muscles and reduce bladder elasticity, making it harder to control urine flow.
- Menopause brings hormonal changes that can lead to a decline in estrogen levels. This can result in changes to the urinary tract, including reduced muscle tone and vaginal dryness, contributing to incontinence.
- In men, an enlarged prostate gland (benign prostatic hyperplasia) can obstruct the urethra and interfere with normal urinary function. This can cause symptoms like urgency and difficulty emptying the bladder, leading to incontinence.
Risk factors for Urinary Incontinence
Below are factors that could increase your likelihood of suffering from urinary incontinence:
Gender
Gender is a significant risk factor for urinary incontinence. Women are more likely to experience urinary incontinence than men. A comprehensive study published in the International Journal of Women's Health (2013) examined this gender disparity. The study found that the anatomical differences in the female pelvic region, such as a shorter urethra and the impact of pregnancy and childbirth, contribute to a higher prevalence of urinary incontinence in women.
Age
Age is a prominent risk factor for urinary incontinence. As individuals age, changes occur in the bladder and pelvic muscles. A longitudinal study published in the Journal of Urology (2008) highlighted the age-related increase in urinary incontinence cases.
Obesity/ Being Overweight
Being overweight or obese is strongly associated with urinary incontinence. A study by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) found a direct correlation between obesity and urinary incontinence. Excess weight places additional pressure on the bladder and pelvic muscles, increasing the risk of incontinence.
Smoking
Smoking is an established risk factor for urinary incontinence. A study published in the American Journal of Obstetrics and Gynecology (2019) explored the relationship between smoking and incontinence in women. The study revealed that smoking can lead to chronic coughing, weakening the pelvic floor muscles, and contributing to urinary incontinence.
Family History
A family history of urinary incontinence can increase an individual's susceptibility. While the exact genetic mechanisms are still under investigation, a 2014 study in the Journal of Urology identified a genetic component in familial cases of incontinence. Genetic factors may influence the structural and functional integrity of the urinary system.
Complications Arising from Urinary Incontinence
Urinary incontinence is more than just an inconvenience; it can have several complications that significantly impact an individual's well-being.
Prolonged exposure to urine can lead to skin problems for individuals with urinary incontinence. The moisture and acidity of urine can irritate and damage the skin, causing conditions like dermatitis or pressure ulcers. These skin problems can be uncomfortable, painful, and prone to infection. Proper hygiene and skin care are essential to prevent such complications.
Urinary incontinence can increase the risk of urinary tract infections. When urine is retained in the bladder for extended periods or when there is incomplete emptying due to incontinence, it provides a breeding ground for bacteria. A UTI can cause symptoms such as frequent urination, a burning sensation during urination, and even fever. Recurrent UTIs can be a significant concern for incontinent individuals requiring medical attention.
The emotional and social consequences of urinary incontinence should not be underestimated. Living with the condition can lead to embarrassment, anxiety, and a reduced quality of life. Individuals with incontinence may avoid social activities, intimate relationships, or travel due to fear of accidents. This can lead to isolation and a negative impact on mental health.
Diagnosing Urinary Incontinence
Diagnosing urinary incontinence is a crucial first step in managing this condition effectively. There are various diagnostic methods and tests that healthcare professionals can use to determine the underlying causes and develop a tailored treatment plan.
Urinalysis
Urinalysis is one of the initial diagnostic tests for urinary incontinence. It involves analyzing a urine sample to check for signs of infection, blood in the urine (hematuria), or other abnormalities. Urinalysis helps identify potential underlying causes of incontinence, such as urinary tract infections or bladder stones.
Cystoscopy
Cystoscopy is a procedure in which a thin, flexible tube with a camera at the end (cystoscope) is inserted into the urethra and guided into the bladder. This allows healthcare providers to visually inspect the bladder's lining and urethra for abnormalities, such as tumors, stones, or signs of inflammation. Cystoscopy can provide valuable information about structural issues contributing to incontinence.
Physical Exam
A comprehensive physical exam is essential for evaluating urinary incontinence. During the exam, your healthcare provider may ask questions about your medical history, including any previous surgeries or medical conditions that could be relevant. They may also perform a physical examination, including assessing the pelvic area, to check for signs of pelvic organ prolapse or muscle weakness that could contribute to incontinence.
An ultrasound of your bladder
An ultrasound of your bladder is a non-invasive imaging test that uses sound waves to create images of the bladder and its contents. This test can help determine if there are any structural abnormalities in the bladder, such as tumors or issues related to bladder emptying.
Stress Test
A stress test is specifically designed to assess stress incontinence, which is the leakage of urine that occurs during physical activities like coughing, sneezing, or lifting. During this test, you may be asked to perform activities that trigger stress incontinence while your healthcare provider observes for any leakage.
Treatments To Improve Pelvic Floor Muscle Function
Physical therapy offers a range of effective treatments for urinary incontinence, mainly if it is related to pelvic floor muscle issues.
Pelvic Floor Exercises
Pelvic floor exercises, often called Kegel exercises, are a series of controlled contractions and relaxations of the muscles that support the bladder, rectum, and uterus (in women). These muscles, collectively known as the pelvic floor muscles, are crucial for maintaining urinary and bowel control.
Like any other muscle group, the pelvic floor muscles can be strengthened through targeted exercises. A stronger pelvic floor provides better support for the bladder and urethra, reducing the risk of leakage.
Pelvic floor exercises enhance your ability to control these muscles. This control is essential for preventing urine leakage during activities that stress the bladder, such as sneezing, laughing, or lifting.
Performing pelvic floor exercises correctly is essential to reap their full benefits. Here's a step-by-step guide:
- Locating the pelvic floor muscles. An effective method is trying to halt the flow of urine mid-stream during a restroom visit—the muscles you engage for this are your pelvic floor muscles.
- Empty your bladder to ensure comfort during the exercises.
- Perform pelvic floor exercises while lying down, sitting, or standing—opt for the most comfortable position.
- Visualize the action of stopping the flow of urine. Squeeze your pelvic floor muscles, feeling a lifting sensation. Avoid tightening your abdomen, buttocks, or thighs.
- Maintain the contraction for three to five seconds, then release. Repeat this process ten times consecutively.
- Do not hold your breath while performing pelvic floor exercises. Maintain steady, relaxed breathing throughout the routine.
- Over time, gradually increase the duration of contractions and the number of repetitions. Your physical therapist will guide your progression based on your individual needs.
Biofeedback
Biofeedback is a fascinating technique employed by physical therapists to help individuals harness the power of their bodies. It is a non-invasive method that unveils the inner workings of your muscles, allowing you to gain control over them in a way you never thought possible.
Biofeedback involves using specialized equipment equipped with sensors or electrodes. These sensors are strategically placed on or near your pelvic floor muscles. They detect and measure the electrical activity generated by these muscles during contractions.
Biofeedback allows your physical therapist to tailor your pelvic floor muscle exercises precisely to your needs. They can monitor the strength and duration of your muscle contractions, making it possible to adjust your exercises for optimal results.
You and your physical therapist can track your progress as you continue with biofeedback-assisted exercises. This objective data allows you to see the improvements in muscle strength and control, which can be highly motivating.
Medications
Medical interventions aim to alleviate incontinence symptoms and underlying causes, offering relief and improved quality of life for those affected.
-
Anticholinergics
Anticholinergic medications are among the most commonly prescribed drugs for treating urinary incontinence, particularly in cases of urge incontinence. They work by blocking the action of acetylcholine, a neurotransmitter responsible for signaling the bladder muscles to contract. By inhibiting these contractions, anticholinergics help increase bladder capacity and reduce the urgency to urinate.
One notable medication in this category is Oxybutynin (Ditropan). It has a long track record of effectively managing urinary urgency and frequency. However, consulting with a healthcare professional regarding potential side effects and individualized dosing is essential.
-
Mirabegron (Myrbetriq)
Mirabegron, or Myrbetriq, offers an alternative approach to managing urge incontinence. Unlike anticholinergics, which inhibit contractions, Mirabegron relaxes the bladder muscles. This medication is particularly well-suited for individuals who may experience adverse effects from anticholinergic drugs or have contraindications.
-
Alpha Blockers
Alpha-blockers, such as Tamsulosin (Flomax), are primarily prescribed for men with urinary incontinence linked to an enlarged prostate (benign prostatic hyperplasia). These medications relax the prostate and bladder neck muscles, improving urine flow and reducing symptoms like dribbling and incomplete emptying of the bladder.
-
Topical Estrogen
Topical estrogen may be recommended for women experiencing stress incontinence due to hormonal changes. Estrogen creams or patches can help restore tissue tone and elasticity in the urethra and vaginal area, ultimately enhancing continence.
Medical Devices
The management of urinary incontinence often involves the use of medical devices, for example:
- Urethral Insert. Urethral inserts are small, tampon-like devices inserted into the urethra to block urine leakage during activities that may trigger incontinence. These devices are discreet and can be used as needed. However, they require proper placement and removal.
- Pessary. Urethral inserts are small, tampon-like devices inserted into the urethra to block urine leakage during activities that may trigger incontinence. These devices are discreet and can be used as needed. However, they require proper placement and removal.
Surgery for Urinary Incontinence
You could opt to undergo surgery should all other treatment options fail.
-
Prolapse Surgery
Prolapse surgery addresses pelvic organ prolapse, where pelvic organs, such as the bladder, rectum, or uterus, descend into the vagina. This descent can lead to urinary incontinence. Prolapse surgery involves repositioning and securing prolapsed organs to their normal anatomical positions. This can alleviate pressure on the bladder and improve continence.
-
Artificial Urinary Sphincter
The artificial urinary sphincter is a device implanted to control urinary flow. It is commonly used to treat severe urinary incontinence, particularly in men after prostate surgery. The surgeon places the artificial urinary sphincter around the urethra. By squeezing the device's pump, the patient can temporarily close the sphincter and prevent urine leakage.
Find a Las Vegas Physical Therapist Near Me
Urinary incontinence, though challenging, can be effectively managed. This guide has illuminated the various facets of this condition, including types, causes, risks, complications, and diagnosis.
For stress incontinence, pelvic floor exercises and consultation with a pelvic health physical therapist can greatly improve control and confidence. Those with urge incontinence in Las Vegas can explore medications like anticholinergics or Mirabegron for relief.
Medical devices provide discreet solutions during activities, preventing unexpected leaks. And if you are seeking long-term relief, surgery is an option. Seek professional guidance, contact an experienced physical therapist, and explore personalized treatments.
We will diagnose your condition at Suarez Physical Therapy and review your medical history. And suggest the ideal treatment for your urinary incontinence problem. Contact us at 702-368-6778 today.