Losing your knee due to disease or unintentional injuries can have a significant impact on your health, emotions, relationships, career, and overall way of life. The recovery process for a patient undergoing an above-knee amputation may require a substantial amount of effort and time. In contrast, other surgical procedures may allow for a quicker return to health and fitness.
When possible, the rehabilitation process for individuals undergoing transfemoral amputation begins before the surgical procedure. Our team of physiotherapists at Suarez Physical Therapy in Las Vegas can assist you in living a better life through patient education, hands-on therapy, and personalized movement recommendations. Schedule an evaluation with our skilled physical therapists today.
An Overview of Above-Knee Amputation
A transfemoral (above-knee) amputation is a surgical procedure performed to remove a lower limb that has experienced severe damage due to illness, accidents, or congenital abnormalities. The primary causes of such amputations are peripheral vascular disease, often associated with diabetes, or serious circulatory disorders affecting the lower limb. Insufficient blood flow hampers the body's ability to heal and mount an immune response against further damage.
Ulcers on the legs or feet may persist and not heal, potentially leading to infection. If left untreated, the infection could spread to the bones, posing a life-threatening situation. To prevent the infection from spreading and eliminate the diseased tissue, amputation becomes necessary. In cases where there is inadequate blood flow to the lower leg or the infection is severe, preventing a below-the-knee surgery, transfemoral amputations are performed.
If a transfemoral procedure is necessary, it is often performed by an orthopedic or vascular surgeon. The goal is to remove the affected or severely injured part of the limb while preserving as much of the healthy bone and tissue as possible. To ensure optimal function of a prosthetic leg after recovery, the surgeon will mold the residual limb.
A transfemoral amputation may be necessary due to the following conditions:
- Diabetes.
- Peripheral vascular illness.
- Infection or gangrene.
- Trauma can lead to a lower leg that’s shattered or crushed.
- Cancer or tumor.
Anatomy of Transfemoral Amputations
The surgeon must know the primary neurovascular structures in the thigh to locate and ligate them. The main artery that supplies the femur and thigh is the femoral artery. Its position may vary depending on the level of amputation, as its course changes along the length of the femur.
There are three chambers in the thigh:
-
High Above-Knee Amputation
The femoral artery is located anteriorly to the femur, below the sartorius muscle, and in front of the adductor longus muscle. The adductor longus muscle is located anterior to the profunda femoris artery. At this point, the femoral vein and artery are positioned laterally to each other. The sciatic nerve is located anterior to the long head of the biceps and posterior to the adductor magnus.
-
Midfemur Above-Knee Amputation
The femoral artery is situated medially to the femur in the mid-thigh region, positioned between the adductor magnus and the vastus medialis. In this same area, the femoral vein can be found laterally to the artery. Additionally, the sciatic nerve is located between the semimembranosus and the short head of the biceps.
-
Amputation Above-Knee Supracondylar
The femur is located directly behind the femoral artery. After traveling through the Hunter canal, the femoral artery enters the sciatic nerves in the popliteal fossa. The artery is situated medially to the sciatic nerve and is deep.
How a Physical Therapist Can Help
Before undergoing a transfemoral procedure, your physical therapist might:
- Offer preoperative conditioning activities that aim to strengthen and limber both the lower and upper extremities.
- Provide instructions on how to walk using crutches or a walker.
- Inform you on what to anticipate following the procedure.
After Surgery
It is recommended that you plan on staying in the medical facility for a period of five to fourteen days after surgery. In addition to having your wound wrapped, you may also have a drain at the surgical site. Rest assured, we will provide medication to effectively manage any post-operative pain you may experience.
After your surgery, physical therapy will commence once your condition stabilizes and your doctor gives the green light for the resumption of your rehabilitation. A physical therapist will visit you at your bedside to discuss your surgery and medical history.
During the initial two to three days of your treatment, you may experience:
- Perform range-of-motion and gentle stretching exercises.
- Acquiring the skills to roll over in bed, sit on the side, and move safely to a chair.
- Acquiring knowledge on proper placement of your surgical limb is crucial to avoid contractures, which refer to the inability to fully extend the knee joint due to excessive flexion of the limb.
The physiotherapist will assist you in learning how to stand and walk with the help of an assistive device, such as a walker, and navigate with a wheelchair once you are medically stable.
Preventing Contractures
When soft tissue becomes tight and limits joint movement, it is referred to as a contracture. This syndrome occurs when soft tissues and muscles become stiff due to inactivity. For example, the hip muscles of an individual who has undergone a transfemoral amputation may become stiff from prolonged sitting in the same position.
Repeatedly lying flat with a pillow between your legs for extended periods may cause a condition called contracture, where your leg extends too far out to the side. Failure to address contractures following surgery, during recuperation, and after therapy can result in long-term damage. Contractures often hinder mobility and the use of prosthetics, making assistance devices like walkers necessary.
Your physiotherapist will assist you in maintaining a normal hip range of motion and posture. They will teach you positioning and stretching exercises to preserve a healthy range of motion and guide you on how to position your limb to prevent the development of contractures.
Compression Therapy for Swelling
It is common to experience swelling after surgery. Your physical therapist will guide you in applying compression to your residual limb to protect it, manage edema, and promote healing.
One way to achieve compression is by
- Applying elastic bandages to the affected limb.
- Putting on an elastic sock shrinker.
These techniques help shape the limb to prepare it for fitting the prosthetic leg. Elastic bandages may not always be required; in some cases, a plaster cast or stiff dressing may be used instead. It is also possible to apply a plaster or plastic immediate postoperative prosthesis.
Since each person's condition is unique, the chosen method will vary accordingly. Your physiotherapist will ensure that these devices fit correctly and provide you with instructions on how to use them effectively.
Pain Control
Your physiotherapist will provide various methods of pain relief assistance, such as:
- The management of pain through the use of electrical stimulation and transcutaneous electrical nerve stimulation (TENS). By preventing nerve impulses from reaching pain receptors, mild electric stimulation of the skin effectively reduces pain.
- Utilizing manual treatment techniques, such as massage and joint manipulation, to improve joint motion and circulation.
- Providing skincare and promoting the appropriate usage of stump socks for the treatment of residual limbs.
- Desensitization technique used in reducing a region's sensitivity to touch or pressure from clothing. The goal is to lessen or eliminate the sensitive reaction to these stimuli. Desensitization involves gently stroking the skin with various forms of touch.
Functional Recovery
The prosthetist and physical therapist will collaborate to determine the ideal prosthesis for your lifestyle and exercise goals. An above-knee prosthesis consists of a knee joint, socket, foot components, and ankle joint. Throughout several months of recovery, your residual limb will continue to heal and shrink or take on the shape of a temporary prosthesis. Your physiotherapist will make the necessary adjustments to ensure a proper fit during this period.
Boosting Independent Performance
Transitioning from acute care to rehabilitation will grant you greater independence in your daily functioning. Your physical therapist will guide you in maneuvering a wheelchair and walking with the assistance of a walker or crutches. They will also teach you the necessary skills to effectively use your prosthetic limb. Additionally, you will learn how to properly care for your remaining limb through skin checks and cleanliness. Exercise and proper placement will help you prevent contractures.
Acquiring Knowledge About Using and Maintaining Prosthetics
You will learn how to put on and take off your new prosthesis from your physical therapist, as well as how to ensure that the socket type you receive fits properly. Your physical therapist will work with you to progressively increase your tolerance for wearing your prosthesis for extended periods while maintaining the integrity of your remaining limb's skin.
Even after receiving a permanent prosthesis, you will still need a wheelchair for mobility during the periods when you are not wearing the prosthetic limb.
The Process of Receiving Prosthetic Training Can Take Up To A Year
Once your doctor gives you the all-clear to start bearing weight on your prosthesis, you can begin your rehabilitation journey. Your physical therapist will provide you with instructions on how to balance, walk, and stand with your prosthetic leg. Initially, you will likely start off using parallel bars and gradually progress to using a walker.
As your strength increases, you may then transition to using a cane before eventually being able to walk independently. It is important to maintain your strength and flexibility to achieve your maximum potential and regain the ability to do many of the things you did before your amputation.
At-Home Self-Care Techniques
To assist in the care of your transfemoral amputation, you can follow these steps:
Activity
- Take action and discuss your options with your physician. Your remaining leg will recover more quickly if you use it and stay active.
- You can take a shower with your doctor's approval. After washing your residual limb with water and soap, make sure to pat it dry. Initially, you may need assistance with this.
- Before driving, you may need to adjust your car to suit your needs.
Once your remaining arm has fully recovered, you should be able to resume work and your regular schedule. This may happen sooner than four to eight weeks following surgery, but it could also take longer.
Nutrition
- You can stick to your typical diet, but if your stomach is unsettled, it's recommended to try bland, low-fat items such as bread, yogurt, broiled chicken, and plain rice.
- Immediately after surgery, it is common to experience irregular stool movements. To avoid constipation and difficult bowel motions, it is recommended to consume a daily fiber supplement. If you haven't had a bowel movement after a few days, it is advisable to consult your doctor about using a mild laxative.
Medication
- You can consult your doctor to find out when and if you can resume taking your medications. Your doctor will provide you with instructions on how to take any new medications.
- Your doctor will advise you on when to resume taking aspirin or another blood thinner if you have previously stopped taking it.
- Adhere to the recommended dosage for pain medication.
- If the doctor has supplied you with prescription pain medication, make sure to take it as directed.
- If you are not already taking a prescription pain reliever, consult your physician to inquire about using an over-the-counter alternative.
- Unless your medical professional has instructed otherwise, take your medication after meals if you feel like it's making you feel ill in your stomach.
- Request a different pain medication from your physician.
It is important to follow your doctor's instructions when it comes to taking antibiotics. Even if you start feeling better, it is crucial not to stop taking them. It is necessary to complete the entire prescribed duration of the medication.
Care for the Remaining Limbs
On the remaining limb, you can have a cast, a stiff dressing, or bandages. Your doctor will guide you on how to take care of it. The specific dressing and instructions will depend on your situation and the doctor's recommendations. These include the following:
- Check for redness, irritation, and any breaks in the skin on the remaining limb. If you notice any issues, be sure to inform your physician.
- Every night, wash the remaining limb in warm water with a mild soap. Gently pat it dry.
- Remove any temporary prosthetic legs before going to bed.
Exercise
After surgery, rehabilitation involves a series of exercises aimed at retraining your artificial leg and residual limb. To create a fitness regimen tailored to your needs, you will work closely with your physiotherapist and doctor.
Your doctor will provide instructions on the frequency and proper execution of the exercises to ensure you achieve the maximum benefits. Your recovery program will include a variety of workouts. It is important to always follow your therapist's instructions.
Follow-up care is a crucial component of your treatment and security. It is important to schedule and attend all of your visits. If you need guidance, do not hesitate to reach out to your doctor or nurse. Keeping a record of the medications you take and staying informed about your test findings are also smart moves.
Is It Possible to Avoid This Condition or Injury?
Research has it that 60% of vascular amputations can be avoided. The main causes of transfemoral amputation are diabetes-related complications, such as peripheral vascular disease, open wounds, and infection. By preventing and treating diabetes and circulation issues in the lower extremities, the likelihood of developing disorders that require lower-extremity amputations can be significantly reduced.
Ensure that you protect your limbs and feet when you have diabetes by wearing appropriate, well-fitting footwear. This will help you avoid complications. It's crucial to regularly check your feet and lower limbs for any signs of skin issues, such as redness, discoloration, swelling, blisters, scrapes, or open wounds. If you notice any concerns, it is important to contact your physical therapist or primary care physician immediately. One of the main ways to prevent amputation is by avoiding infection.
Giving up smoking is crucial. Cigarette smoking can impede the healing process and increase the risk of re-amputation in smokers by 25 times compared to non-smokers.
What Type of Physiotherapist Do I Require?
Physical therapists are highly qualified to handle issues related to above-knee amputations due to their education and expertise. However, there are a few factors you might want to consider:
- A physical therapist with expertise in caring for patients facing amputation can provide valuable support. Some physical therapists specialize in prosthetic training and rehabilitation for patients who have undergone extremity amputations.
- A physical therapist who has completed a fellowship or residency program in physical rehabilitation can potentially assist you with your issue due to their extensive training, experience, and skills.
General advice for anyone searching for a physiotherapist includes the following:
- Consult with friends, relatives, and other medical professionals for referrals.
- When making an appointment at a physical therapy clinic, you can inquire about the physiotherapists' experience in treating patients who have undergone lower-extremity amputations.
- Provide a detailed description of your symptoms, along with information about what triggers them.
Find a Las Vegas Physiotherapist Near Me
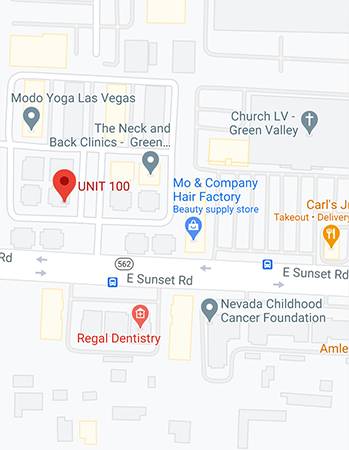
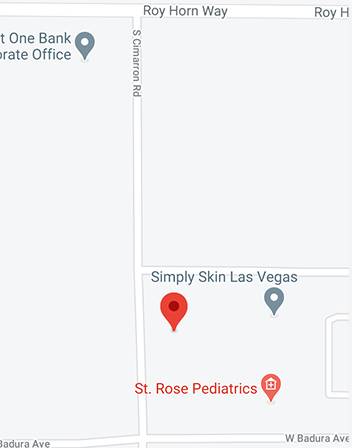
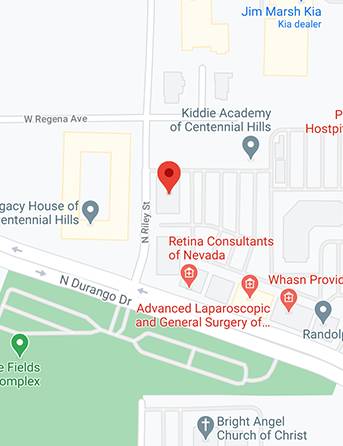
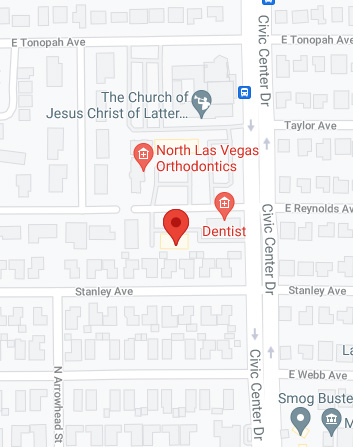
While a transfemoral amputation can certainly have a significant impact on your life, it's important to remember that you don't have to face it alone. With the support of a dedicated physical therapist and rehabilitation team, you can work towards restoring your mobility, independence, and overall well-being. Whether you choose to use a prosthesis or not, the experienced team at Suarez Physical Therapy in Las Vegas is here to provide personalized services tailored to help you achieve your health objectives.
During each session, patients receive manual therapy and are educated on therapeutic modification techniques. Our commitment is to provide quality services, helping you get back to your regular activities and sports as soon as possible. If you have any questions or would like to schedule a session, call us today at 702-368-6778.